For healthcare leaders navigating digital transformation and M&A, an API-first strategy is no longer optional. It is a core driver of organizational value. A well-architected healthcare API ecosystem allows you to scale operations, deliver personalized patient care, and significantly increase your company’s valuation. Organizations with mature API platforms integrate faster post-acquisition, innovate more quickly, and command higher multiples.
Understanding the strategic and technical components of this shift is the first step toward building a future-proof, high-value practice. This guide provides the blueprint.
Why Bother? The Strategic Value of an API Ecosystem vs. Traditional Integration
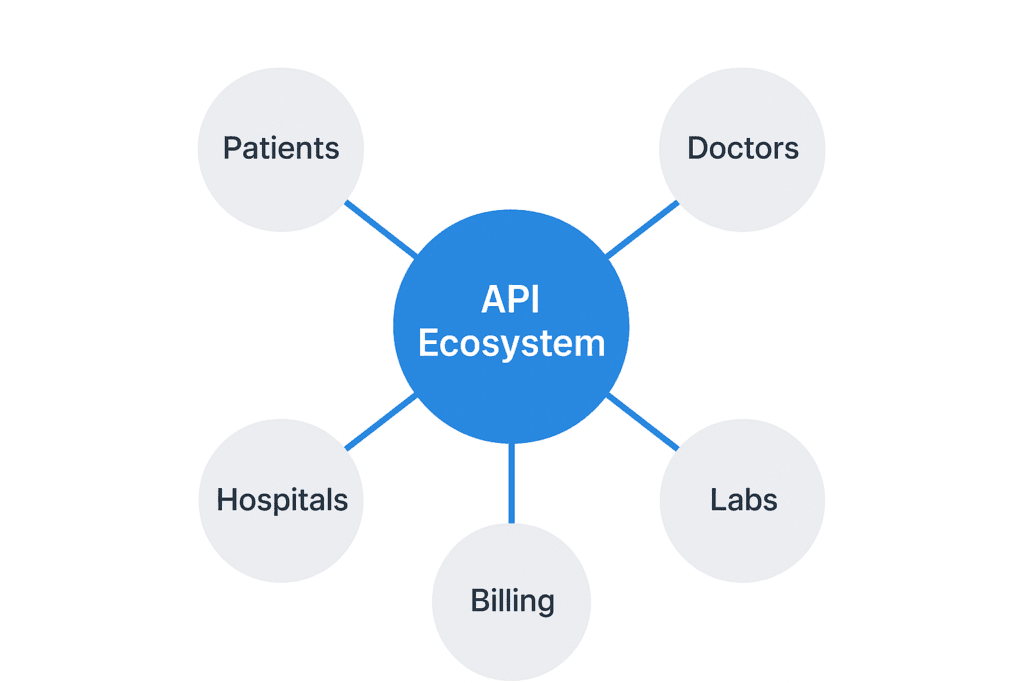
Traditional, point-to-point IT integration creates a brittle and costly web of custom connections. This old model is slow, difficult to maintain, and stifles innovation. A modern healthcare API ecosystem, by contrast, acts as a central nervous system for your organization. It is a flexible, standardized platform for real-time data exchange. This is a fundamental business model shift in the healthcare sector that you should benefit from.
| Traditional Integration | API Ecosystem |
| Rigid, custom connections | Flexible, reusable services |
| Slow, batch data processing | Real-time data access |
| High maintenance costs | Simplified maintenance & governance |
| Difficult to scale | Designed for horizontal scalability |
| Stifles innovation | Accelerates new service development |
“Valuation Insight: Our analysis shows that healthcare organizations with mature API ecosystems command 30-40% higher valuations during M&A transactions. This digital readiness is a critical factor in how to value a medical practice in 2025”
What Are the Building Blocks of a Modern Healthcare API Ecosystem?
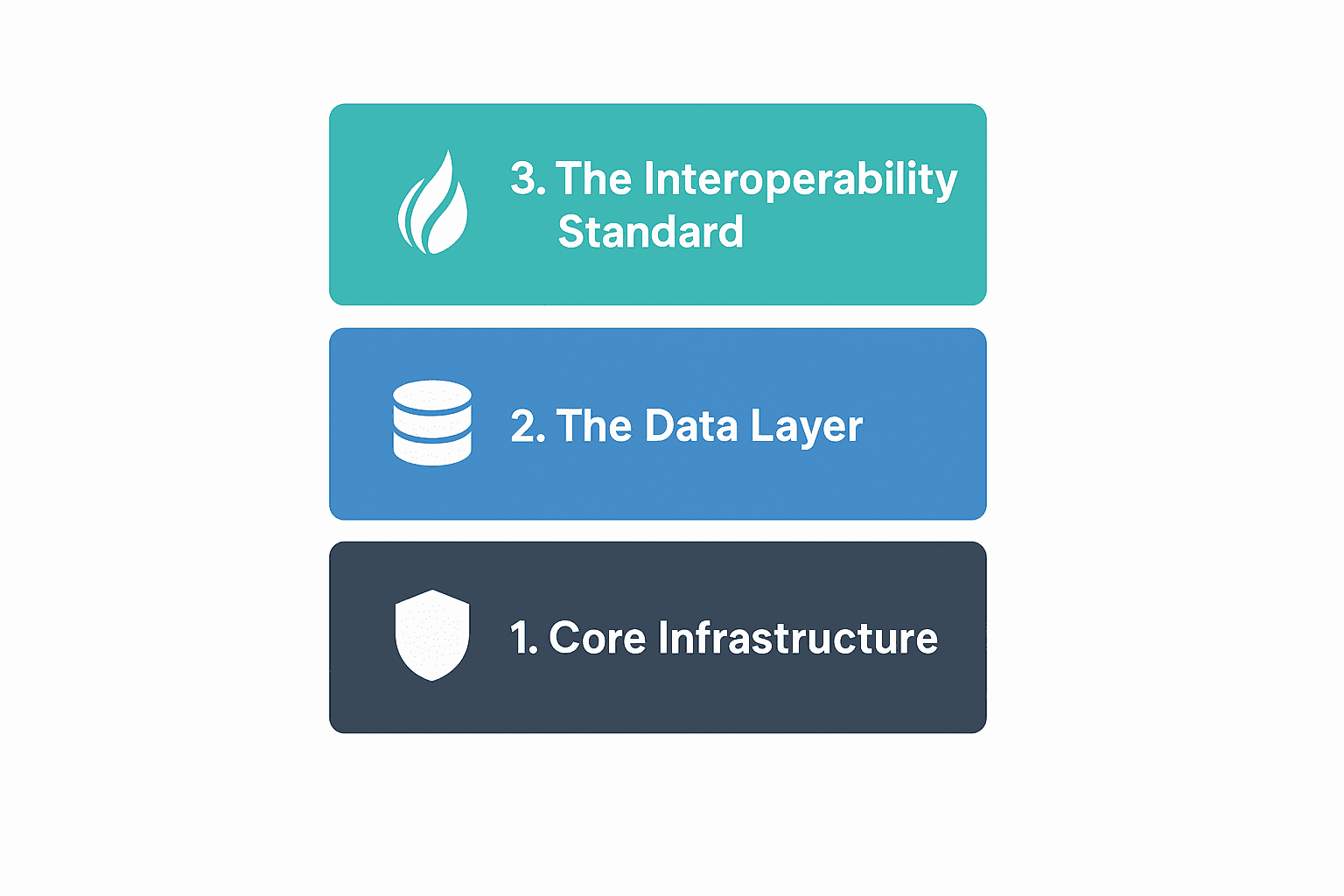
Building a robust ecosystem requires a layered approach. You should think of it as constructing a high-performance facility, starting with the foundation and infrastructure.
1. Core Infrastructure: The Gateway and Service Mesh
This is the operational backbone that manages how all your services communicate.
- An API Gateway acts as the secure front door. It handles critical functions like authentication, traffic management, rate limiting, and monitoring. This ensures only authorized users can access data in a controlled way.
- A Service Mesh manages the complex communication between your internal microservices. It provides service discovery, load balancing, and fault tolerance like circuit breakers, ensuring the system remains resilient even if one component fails.
2. The Data Layer: Smart, Compliant Storage
A one-size-fits-all database is no longer sufficient. A modern data layer uses a “polyglot persistence” strategy, which means choosing the right tool for the right data type. This includes using reliable relational databases for structured clinical data, scalable object storage for medical images, time-series databases for real-time IoT data, and flexible NoSQL databases for documents and notes. Critically, a Master Data Management (MDM) strategy is essential to ensure a single source of truth for patients, providers, and facilities. Without it, your APIs will only serve fragmented, unreliable data.
3. The Interoperability Standard: FHIR (Fast Healthcare Interoperability Resources)
FHIR is the universal language of modern healthcare data exchange. Built on modern web standards like REST and JSON, it provides a consistent, globally recognized model for representing clinical information. This is a core component of the 2025 healthcare interoperability standards that all practices must now navigate.
Instead of a disruptive “rip-and-replace” project, you can implement FHIR facades over existing legacy systems. This approach allows you to gradually expose data through a standard interface, accelerating interoperability without halting current operations. Start with high-value resources like Patient, Practitioner, Encounter, and Observation.
How Do You Build a System That’s Both Scalable and Personalized?
The goal is mass customization, a system that can serve millions of patients while treating each one as an individual. This is achieved through smart architectural design.
Separate Core Services from the Personalization Layer
Decouple your architecture to allow for independent scaling.
- Base Services are the scalable, high-throughput workhorses of your system. Think of appointment scheduling, lab result retrieval, and insurance verification. These can be scaled horizontally to handle massive load.
- The Personalization Layer sits on top, applying patient-specific rules and preferences. It handles care plan customization, clinical protocol adaptation, and communication preferences.
This separation allows you to deliver a unique experience for every patient without compromising the performance of your core infrastructure.
Organize Around Clinical Domains, Not Technology
Structure your APIs using Domain-Driven Design (DDD). Instead of generic “data” APIs, build microservices around specific business and clinical functions. Examples include Patient Management, Clinical Encounters, Revenue Cycle management for specialties like urology, and Population Health analytics.
M&A Insight:In our experience facilitating acquisitions, organizations using a domain-driven architecture complete technical integrations up to 60% faster than those with tangled, monolithic systems. This addresses many common technology and EMR integration challenges.
How Do You Ensure Security and HIPAA Compliance?
In healthcare, security is not a feature but a prerequisite for existence. Adhering to robust healthcare cybersecurity frameworks is the first step. You must go beyond basic protections by implementing a “privacy by design” framework.
Adopt a Zero Trust Security Model
The old “trust but verify” model is dead. You should assume no user or service is trusted by default.
- Verify Everything by implementing strong authentication with OAuth 2.0 and SMART on FHIR. You must also enforce multi-factor authentication (MFA).
- Enforce Least Privilege using Role-Based (RBAC) and Attribute-Based (ABAC) access controls. This ensures users and systems can only access the minimum data necessary. For an acquiring entity, this is a key part of navigating Stark Law and Anti-Kickback statutes
- Protect Your Data with end-to-end encryption for data in transit and at rest. Implement robust audit logs that track every single access and modification to Protected Health Information (PHI).
Important:Organizations with a well-documented API security program and certifications like HITRUST or SOC 2 often see faster M&A deal closures and may benefit from lower cyber insurance premiums.
Manage Third-Party Risk Diligently
Your ecosystem is only as secure as its weakest link. Establish a rigorous framework for onboarding and managing third-party developers and partners. This vetting process is a crucial part of building your complete healthcare M&A advisory team, as technology partners are as critical as legal or financial ones.
What’s the ROI? Measuring the Success of Your API Ecosystem
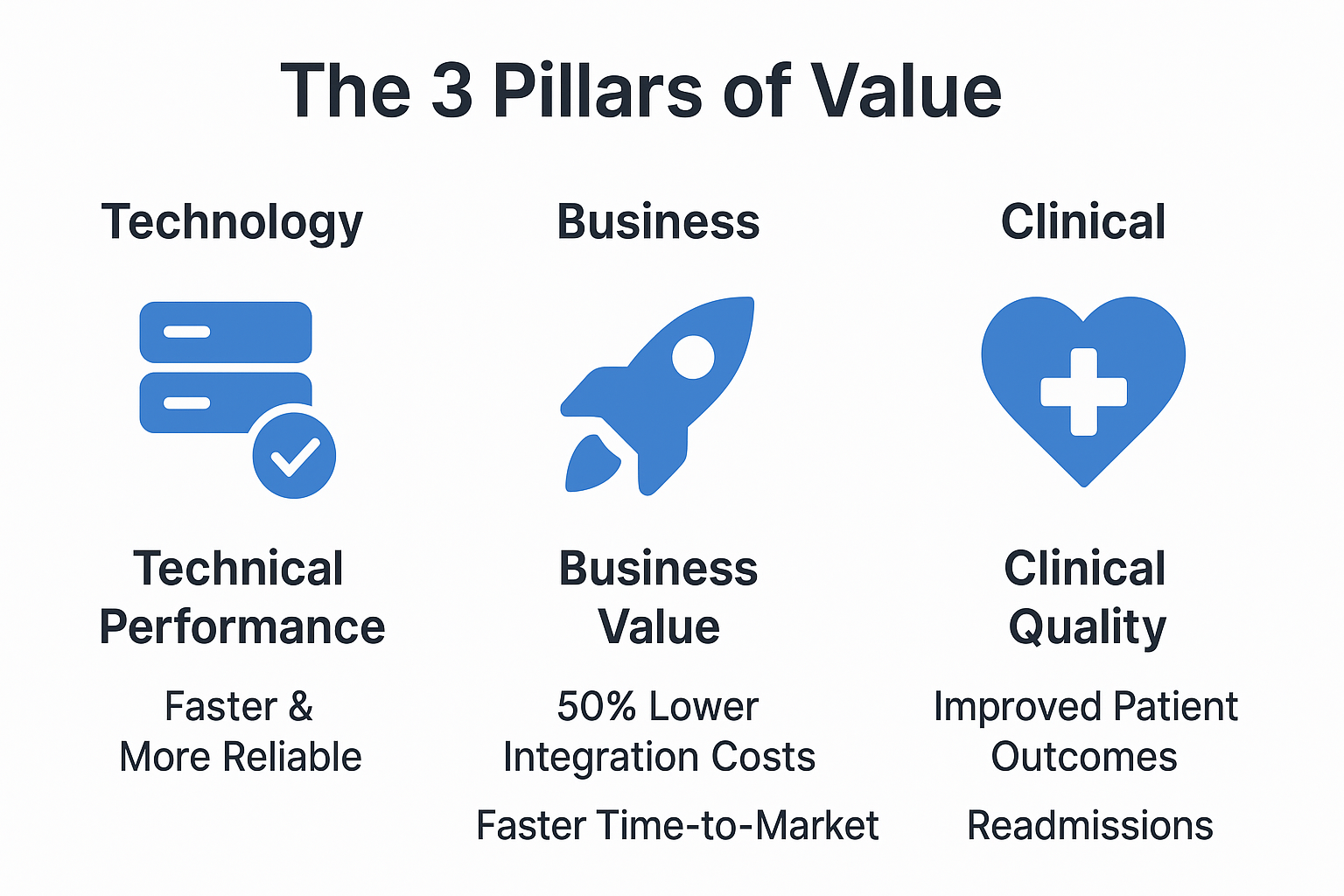
To justify continued investment, you must measure success across technical, business, and clinical domains.
1. Technical Performance Metrics
These KPIs ensure your system is reliable and performant. Key metrics include API uptime, mean time to recovery (MTTR), API response time (P95 latency), throughput, and error rates.
2. Business Value Indicators
This is where your investment pays off. Track the decrease in integration cost per partner, the time it takes to launch new digital services, and the growth of active API consumers and call volume.
These metrics are central to calculating the return on investment for any new technology, a process detailed in our patient engagement platform ROI analysis. Organizations with mature API programs regularly report 50% reductions in integration costs and 70% faster time-to-market for new digital health tools.
3. Clinical Quality Improvements
Ultimately, the goal is better patient care. Correlate your API-enabled workflows with improvements in readmission rates, medication adherence, and clinician efficiency. These outcomes are often enhanced by tools like AI clinical decision support systems (CDSS).
Position Your Technology for a Successful Transaction
The strength of your healthcare API ecosystem is a defining factor in your practice’s valuation and strategic opportunities. This technical infrastructure is no longer a simple line item but a core asset that sophisticated buyers and investors actively seek.
As top M&A advisors, our role is to translate these complex technical assets into a clear, compelling valuation story for investors and acquirers. We demonstrate how a robust API platform enhances operational efficiency, accelerates growth, and significantly de-risks post-acquisition integration for a potential partner.
If you are preparing for a sale or exploring a strategic partnership, understanding how your digital maturity will be perceived by the market is a critical first step.
Contact our team for a confidential consultation to assess how your technology impacts your M&A readiness and overall valuation. To learn more about preparing your practice for a premium outcome, read our guide on how to maximize the valuation of your healthcare practice before selling.



