
If you’re a healthcare executive wrestling with outdated compensation structures while facing mounting pressure from value-based contracts, you’re not alone. Clinical compensation model transformation has become a strategic imperative as healthcare organizations navigate the shift from volume-based to value-based care, yet most struggle with where to begin and how to implement change effectively.
The stakes couldn’t be higher. With 50% of medical groups now tying physician compensation to quality metrics and the value-based care market projected to exceed $1 trillion, organizations that delay transformation face financial instability and competitive disadvantage.
Key Insight: Organizations approach the financial tipping point when 40% of revenue comes from value-based payments, making compensation redesign essential for survival.
What Does Compensation Modeling Mean in Healthcare?
Compensation modeling is the systematic process of designing, analyzing, and implementing physician payment structures that align individual performance with organizational goals and external reimbursement models. In today’s healthcare environment, an effective compensation strategy must balance attracting talent, ensuring financial sustainability, meeting regulatory requirements, and improving patient outcomes.
Your compensation model becomes the primary mechanism for translating organizational strategy into physician behavior. When external payment models shift toward value-based arrangements but internal compensation remains volume-focused, you create a fundamental misalignment that threatens both financial performance and physician satisfaction.
Critical Warning: Misaligned compensation models can cost health systems over $300,000 annually per employed physician beyond generated revenue.
Understanding the Main Types of Compensation Strategies
Today’s clinical compensation models fall into four primary categories:
Salary-Based Compensation
Pure salary models provide predictable income and promote collaborative care delivery. Kaiser Permanente’s success demonstrates this model’s potential, though you’ll need strong performance management systems. The key advantage is alignment with value-based care objectives.
Productivity-Based Models
Traditional productivity compensation ties income directly to wRVU generation or gross collections. While effective in fee-for-service environments, these models become problematic as organizations assume financial risk under value-based contracts. Pure productivity models are increasingly difficult to sustain.
Hybrid Compensation Structures
The most common approach combines base salary (60-70%), productivity incentives (20-25%), and performance bonuses (10-15%). This structure provides income stability while maintaining motivation for both volume and value. MGMA reports this as the predominant model among successful health systems.
Value-Based Compensation Models
Fully value-based models tie the majority of income to patient outcomes, cost management, and quality metrics. These structures align with ACO arrangements but require sophisticated data infrastructure and physician buy-in. Implementation typically starts with shadow periods.
Industry Trend: MGMA data shows quality-tied compensation grew from 26% of groups in 2016 to 50% in 2024.
The Strategic Imperative for Clinical Compensation Model Transformation
Your organization faces converging pressures making transformation essential. The average employed physician costs health systems over $300,000 annually beyond generated revenue, creating unsustainable economics under traditional volume-based compensation.
CMS has established a goal of 100% of Traditional Medicare beneficiaries in accountable care relationships by 2030. MIPS applies payment adjustments from -9% to +9% based on performance. Beginning in 2026, physicians in Advanced Alternative Payment Models receive higher updates than those in traditional fee-for-service.
With 70% of physicians now employed rather than in private practice and a projected shortage of 86,000 physicians by 2036, you must offer competitive, transparent compensation to attract and retain talent.
Regulatory Reality: Beginning in 2026, value-based care participants will receive 0.75% payment updates versus 0.25% for traditional fee-for-service physicians.
Implementing Your Compensation Transformation Strategy
Successful transformation requires a systematic, phased approach:
| Phase | Duration | Key Activities | Success Metrics |
| Assessment & Design | 3-6 months | Current state audit, physician engagement, FMV analysis | 60% physician committee participation |
| Pilot & Shadow | 6-12 months | Test new models, communication campaigns, metric refinement | Physician understanding scores >80% |
| Gradual Implementation | 2-3 years | Phased rollout, monitoring, adjustments | <5% annual compensation reduction |
Begin with comprehensive analysis of current arrangements. You would likely discover a wide array of different pay practices. Engage physician leaders early, with 60% physician involvement in methodology development proving optimal.
Also implement shadow periods where physicians see projected earnings without financial impact, and invest heavily in communication through town halls, updates, and online resources explaining the strategic rationale.
Implementation: Organizations with successful transformation include physician champions who can set aside departmental concerns for enterprise goals.
Technology Infrastructure for Modern Compensation Models
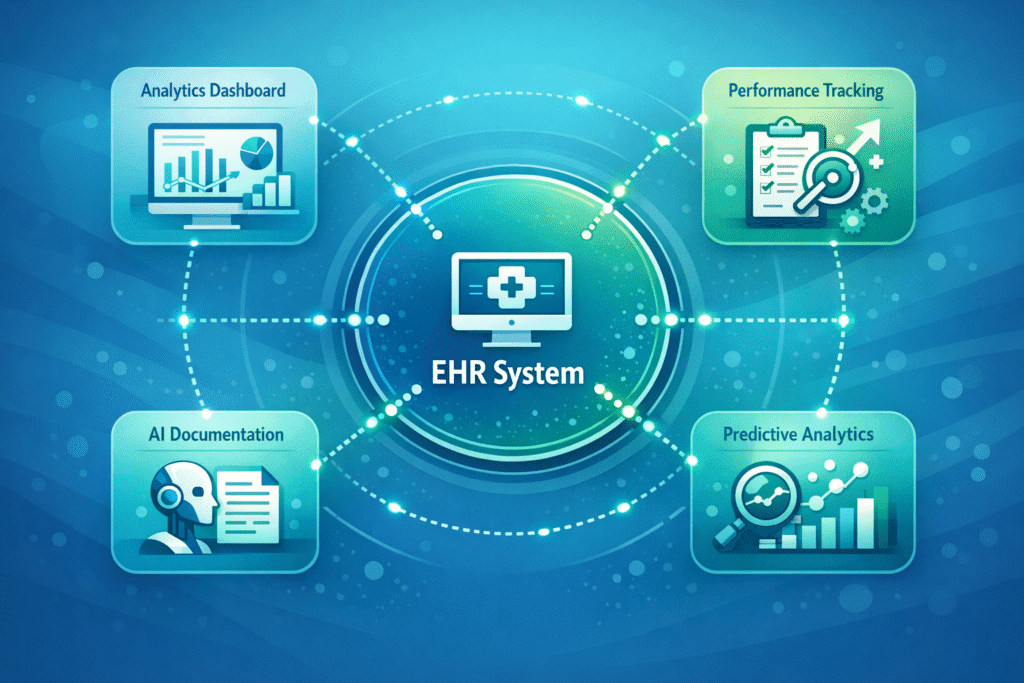
Modern clinical compensation models require integrated systems tracking physician performance across multiple dimensions in real-time. Essential components include EHR-integrated performance tracking for patient attribution and quality metrics, plus data analytics platforms processing clinical, claims, and social determinant data.
Organizations report that real-time interoperability implementation reduces administrative burden by 30% and improves financial transparency. AI-enabled ambient documentation tools cut physician documentation time by 75%, while predictive analytics identify performance trends for proactive intervention.
Tech Reality: 93% of large practices seeking new systems want integrated solutions with AI, analytics, and value-based care support.
Measuring Success of Clinical Compensation Model Transition
Your compensation strategy success should be measured across multiple dimensions. Track financial metrics like physician cost per wRVU and MGMA benchmark alignment, clinical quality metrics aligned with value-based contracts, and physician satisfaction surveys.
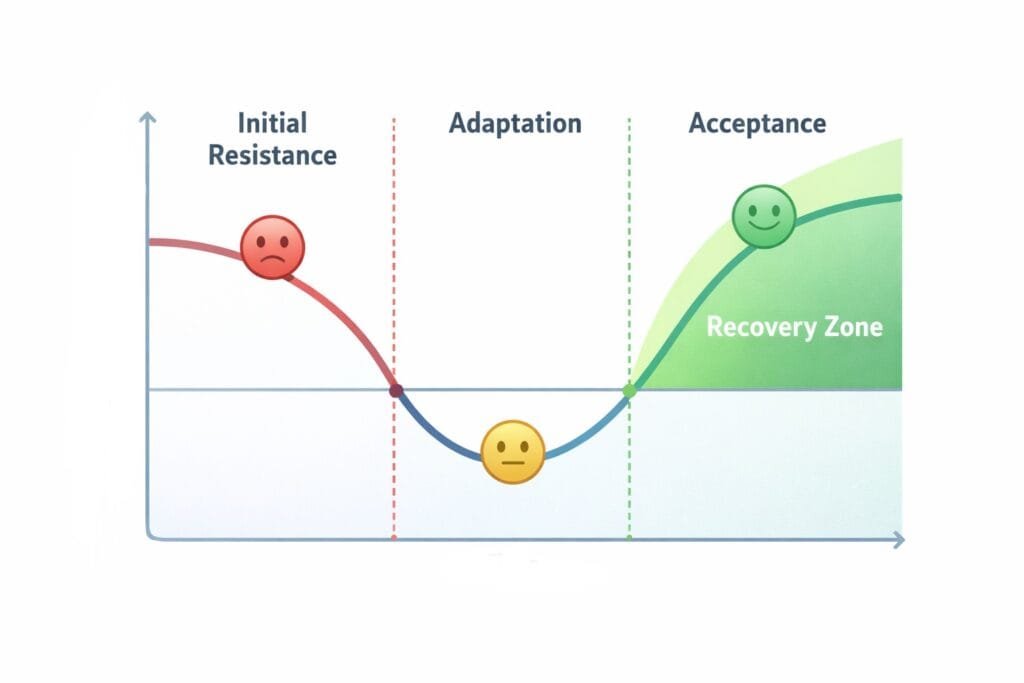
Organizations achieving sustainable transformation typically see initial satisfaction dips followed by recovery as physicians adapt. Long-term sustainability requires annual reviews assessing metric relevance, benchmark alignment, and regulatory requirements.
Regulatory compliance also remains critical throughout transformation. Work with experienced healthcare attorneys to structure compliant arrangements. The most successful organizations achieve simultaneous improvement in clinical metrics and physician satisfaction, while achieving regulatory compliance.
Transforming your Clinical Compensation Model
Organizations mastering clinical compensation model transformation position themselves competitively for the next decade, while those delaying face mounting financial pressure and workforce challenges.
SovDoc’s healthcare M&A experts have guided organizations through successful compensation transformations nationwide. Our team understands the unique financial, regulatory, and operational challenges you face in today’s evolving healthcare environment. We provide comprehensive assessment, strategic design, and implementation support that ensures your transformation achieves both financial objectives and physician satisfaction.
Contact SovDoc today to discuss your specific situation and develop a customized compensation transformation approach. Your organization’s financial sustainability and competitive position depend on getting this right, and you don’t have to navigate it alone.



