If you’re managing a medical practice or considering acquisition opportunities, you’ve likely noticed the dramatic shift in how healthcare organizations deploy advanced practice providers. With physician shortages projected to increase and APPs representing the fastest-growing segment of the healthcare workforce, understanding integration models is essential for practice sustainability and value.
Whether you’re exploring how to maximize your existing APP investments or evaluating practices with established integration frameworks, the decisions you make today will determine your organization’s competitive position in an increasingly APP-dependent healthcare landscape.
What Are Advanced Practice Provider Integration Models?
Advanced practice provider integration models are structured frameworks that define how nurse practitioners, physician assistants, and other APPs function within your clinical practice and care teams. These models determine workflow patterns, billing strategies, regulatory compliance, and your practice’s financial performance.
Key Insight: Integration models serve as the blueprint for your practice’s operational DNA.
The choice of integration model affects every aspect of your practice operations. With over 461,000 licensed nurse practitioners and 189,907 certified physician assistants now practicing nationwide, getting this framework right is fundamental to practice success.
The Core Integration Models Shaping Modern Clinical Practice
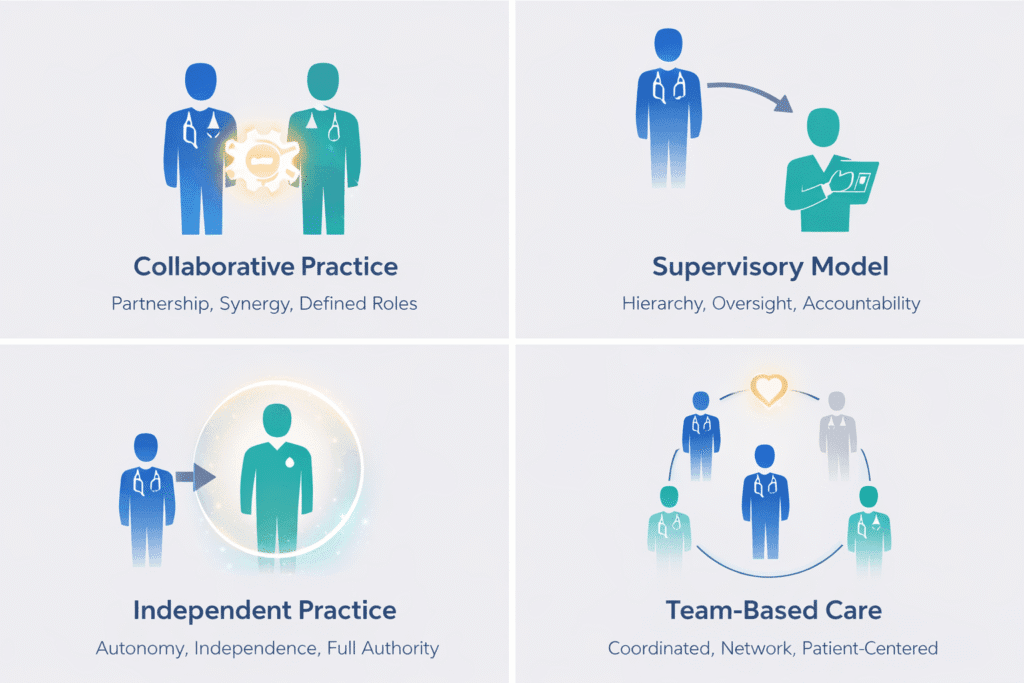
Understanding these four primary integration models will help you make informed decisions about structuring your delivery of care.
Collaborative Practice Models: Shared Responsibility Frameworks
Physicians and advanced practice providers share patient care responsibilities through clearly defined roles and communication protocols. Written agreements specify authorized activities, prescriptive authority, and consultation requirements.
This approach works well in multi-specialty practices with coordination infrastructure. The University of Tennessee Medical Center increased outpatient cardiology encounters by 7.5% after implementing structured collaborative workgroups.
Supervisory Models: Traditional Oversight Structures
Physicians hold direct responsibility for APP clinical activities. While providing clear accountability, these models can create bottlenecks, especially where supervising physicians are scarce. Consider whether your physician capacity can handle supervision requirements without limiting APP utilization.
Independent Practice Models: Maximizing APP Autonomy
This represents the market’s direction. For nurse practitioners, full practice authority means complete diagnostic and prescriptive independence. Currently, 27-34 states plus Washington D.C. grant full practice authority. Eight states have adopted “Optimal Team Practice” frameworks for physician assistants, removing administrative constraints while maintaining collaboration.
Team-Based Care Models: Coordinated Service Delivery
All members practice to their full educational capacity in coordinated units. The Stanford Primary Care 2.0 model showed improved team development, patient satisfaction, and reduced burnout.
What Are the Pillars of an Advanced Practice Framework?
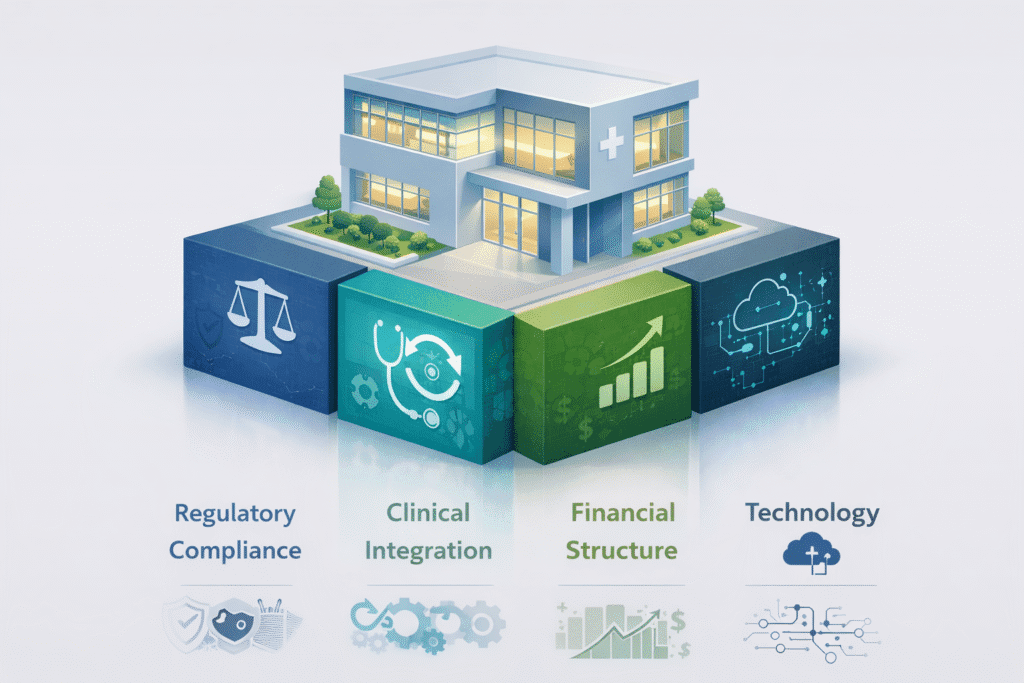
The foundation of successful APP integration rests on four critical pillars that determine whether your integration efforts succeed or struggle. Understanding these pillars will help you evaluate existing practices and design implementation strategies that deliver sustainable results.
| Pillar | Key Focus | Success Metric |
| Regulatory Compliance | State practice authority and billing rules | Zero compliance violations |
| Clinical Integration | Workflow design and role clarity | 85%+ template utilization |
| Financial Structure | Compensation and revenue optimization | $200K+ revenue per APP |
| Technology | EHR integration and performance tracking | Real-time productivity dashboards |
These four pillars work together to create a framework that maximizes APP capabilities while ensuring compliance and financial performance. Organizations that master all four pillars report significantly better outcomes including lower turnover, improved productivity, and enhanced practice valuations.
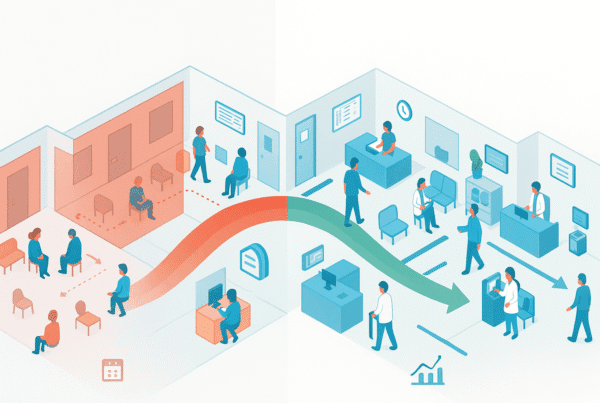
How Do Advanced Practice Models Transform Care Delivery?
Advanced practice providers fundamentally change how your organization delivers clinical services by dramatically improving patient access and capacity. Research shows APPs grew to represent more than 25% of all billed Medicare encounters from 2013 to 2019, with adding an NP or PA increasing practice panel capacity by approximately 600 patients without proportional overhead increases. A 2018 Cochrane Review found nurses provide care equivalent to physicians with similar outcomes, while academic medical centers report Net Promoter Scores of 85.7 for APP-delivered care.
The economics create compelling opportunities for service expansion and improved outcomes. APPs deliver equivalent care at 6-7% lower total costs, with diabetes patients receiving NP/PA care saving $2,626 per patient compared to physician-delivered care. Retail clinics demonstrate this scalability with 1,800 locations across 44 states and market value projected to reach $4-6.36 billion by 2030, positioning practices with strong APP integration advantageously for both value-based contracts and acquisition opportunities.
Implementation Strategies That Drive Success
Implementation success depends critically on executive sponsorship and dedicated leadership for APP integration. Health systems creating dedicated APP leadership roles—Director of Advanced Practice, VP of APPs—report measurably better outcomes including lower turnover, improved productivity, and better physician-APP collaboration.
Effective onboarding and performance management prevent early departures and accelerate productivity. Your onboarding process should include pre-arrival licensure verification, EHR training, compliance education, and defined clinical productivity expectations with a planned 3-6 month ramp-up period. Currently, 97% of practices track individual APP productivity in ambulatory settings, with systematic measurement optimizing APP integration and demonstrating value through clinical productivity, quality metrics, and operational efficiency tracking that prevents costly staff departures before they occur.
Retention Boost: Systematic performance reviews prevent costly staff departures.
Moving Forward with APP Integration
Start by evaluating your current integration across the four pillars: regulatory compliance, clinical integration, financial structure, and technology infrastructure. If you’re considering acquisitions, prioritize practices with demonstrated APP integration capabilities, especially in states with favorable regulatory environments.
SovDoc specializes in helping healthcare organizations navigate the complexities of APP integration through strategic M&A opportunities. Our deep understanding of regulatory environments, financial modeling, and integration best practices enables us to identify high-value acquisition targets and optimize existing APP deployments. Whether you’re looking to enhance your current practice’s APP utilization or acquire practices with established integration frameworks, SovDoc’s healthcare M&A expertise delivers the strategic guidance and transaction support you need to succeed in an APP-dependent healthcare future.