If you’re losing sleep over denied claims eating into your practice’s revenue, you’re not alone. Healthcare providers now spend billions annually to fight claim denials when majority of these denials are completely preventable through proper denial prevention system implementation.
High denial rates stall practice growth and efficiency while also standing in the way of a smooth operational system, but they don’t have to. This guide walks you through everything you need to know to build an effective denial management system and protect your revenue.
Why You Can’t Afford to Ignore Denial Prevention System Implementation?
The average medical practice faces denial rates of 5-10%, with some even struggling with rates as high as 29%. Each denied claim costs between $25-$118 to rework, and that’s if they are resubmitted at all. The shocking truth is that 65% of denials are never resubmitted which simply means pure revenue is walking right out the door. If you are looking to maximize your valuation or simply enhance patient financial experience, then this is a no-no.
Think of it this way: if you’re processing 10,000 claims annually at a 10% denial rate, you’re dealing with 1,000 denied claims. At $50 per claim to rework, that’s $50,000 in administrative costs alone, not even counting the lost revenue from claims you never resubmit. Sounds like a nightmare.
Good News Practices that implement comprehensive denial prevention systems see 15-20% reductions in denial rates within 6-12 months, with many achieving denial rates under 5%.
What Are the Steps of Denial Management?
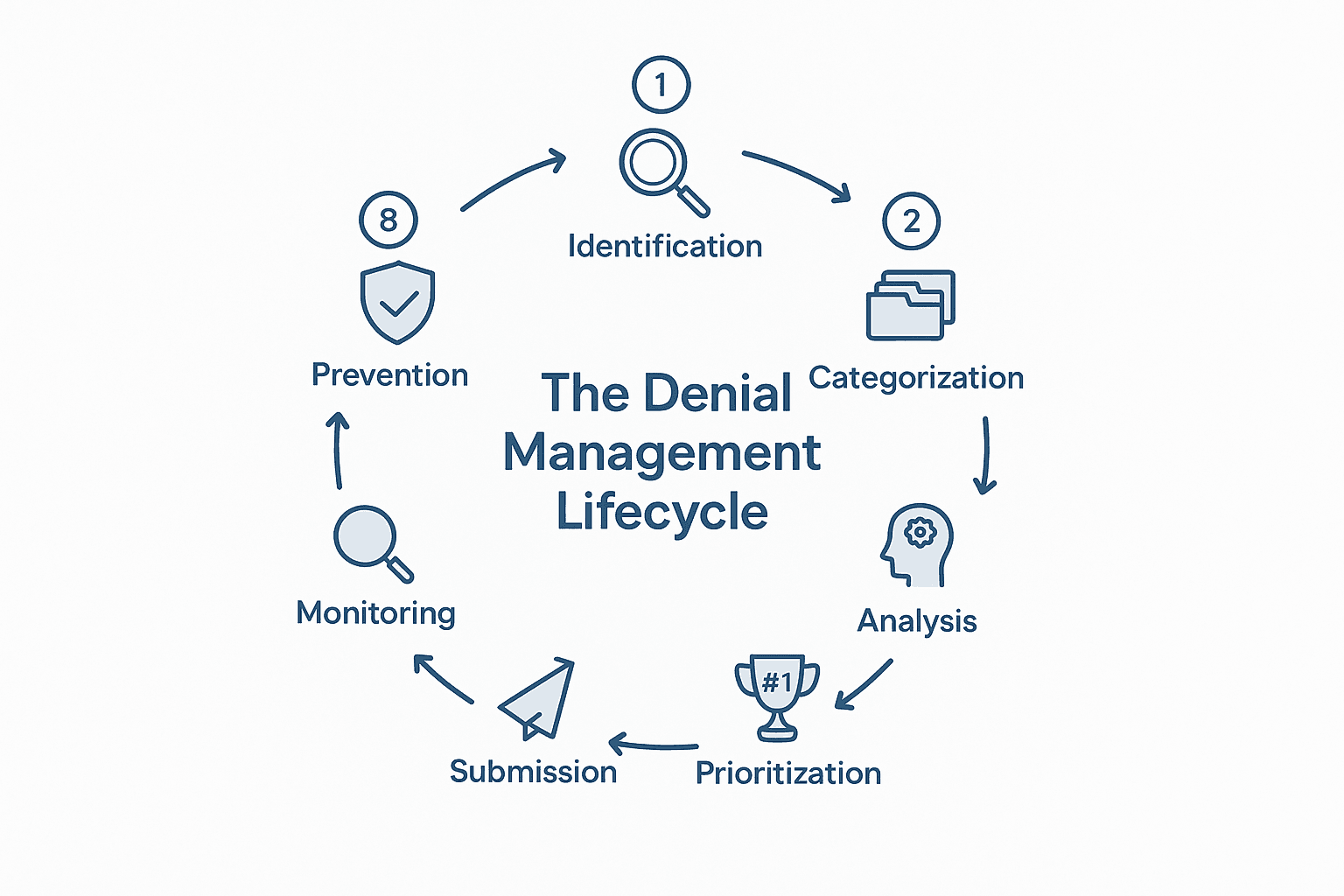
It is important to get a bird’s eye view of denied claims before diving into prevention, and to do so, it is crucial that you understand how an effective denial management process works. The process begins with immediate identification and detection, where denied claims are flagged within 24–48 hours of receiving Electronic Remittance Advice (ERA) or Explanation of Benefits (EOB) documents. Next is categorization by root cause, grouping denials into five main categories: eligibility problems, coding errors, administrative failures, authorization deficiencies, and medical necessity issues. Once categorized, a root cause analysis should be conducted to uncover why the denials occur rather than simply treating their symptoms.
After understanding the underlying issues, the next step is strategic prioritization, focusing first on high-dollar claims nearing their deadlines, as Medicare allows 365 days for resubmission while most commercial insurance payers permit only 90–180 days. Following prioritization comes resolution and correction, where correctable errors are fixed immediately and resubmitted with comprehensive documentation to support appeals. This leads to appeal submission and tracking, ensuring appeals are submitted promptly and monitored closely until resolved.
Finally, performance monitoring is essential—track key metrics such as initial denial rate, time from denial to resolution, and appeal success rates on a monthly basis. The process concludes with prevention implementation, using denial data to proactively prevent future denials rather than addressing them only after they occur.
How Can You Prevent Denials?
Many practices spend 90% of their effort appealing denials and only 10% preventing them. Once you flip this ratio and invest heavily on the front-end, you’ll see dramatic improvements. You can start by implementing optimization strategies to smooth out your revenue cycles and also instill a four-pillar approach (as laid out below) specifically for denial prevention.
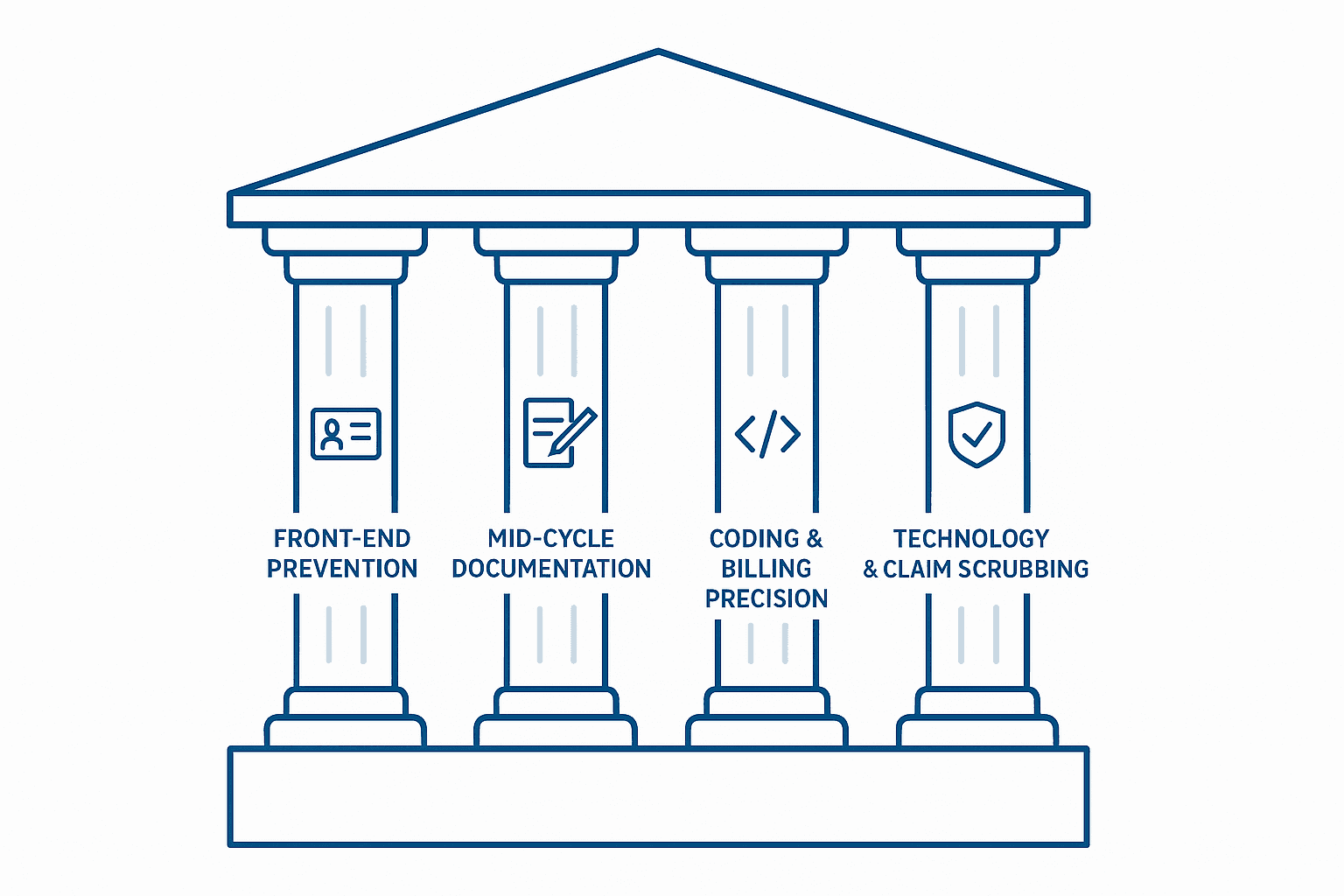
Front-End Prevention
Real-time eligibility verification is the cornerstone of denials prevention. Check every patient’s insurance 24-48 hours before their appointment. You can’t rely on what they tell you because insurance changes constantly. Your automated eligibility checking system should verify active coverage status, plan type and coverage limits, patient financial responsibility, and service-specific coverage.
Prior authorization mastery is equally critical. With 77% of providers reporting that payer policies change more often and 97% experiencing patient delays due to authorization requirements, you need a bulletproof system. Submit authorizations 3-5 business days before service, confirm authorization numbers immediately before procedures, and track expiration dates religiously.
Mid-Cycle Documentation Excellence
Clinical Documentation Improvement (CDI) programs are essential for effective denials management. Organizations with active CDI programs experience 25-30% reduction in claim denials. Your physicians need to document clinical rationale linking diagnoses to treatments, severity and complexity indicators, patient response to treatment, and specific ICD-10 codes supporting medical necessity.
Coding and Billing Precision
Computer-assisted coding with automated edit checks catches errors before submission. Focus on ICD-10 specificity requirements, CPT code accuracy and modifier usage, National Correct Coding Initiative (NCCI) edits, and bundling and unbundling rules. Understanding clean claim rates is also essential for measuring your coding precision effectiveness.
Technology-Enabled Claim Scrubbing
Pre-submission validation using claims scrubbing software guarantees improved clean claim acceptance rates. These systems check for complete patient demographics, valid procedure and diagnosis codes, proper authorization numbers, and coordination of benefits accuracy.
Focus Area: Eligibility problems cause a large portion of denials. This makes real-time eligibility verification your highest-impact prevention strategy.
What Technology Solutions and Team Structure Do You Need?
When evaluating practice management automation tools, modern AI-powered denial management systems should be a priority. These systems predict which claims will be denied before you submit them, analyze historical denial patterns, flag high-risk claims for review, suggest corrections before submission, and help high-performing practices achieve denial rates under 3%. However, it is important for you to note that technology upgrades and implementation require proper training and physician engagement to be effective. Your physicians also create the documentation that supports claims. If they’re not on board with CDI principles, your denial prevention efforts will fall short.You need to build the right team, train them properly on the necessary operation systems and tech, and adopt a structure that accommodates dedicated roles with specific responsibilities and success metrics:
Implementation Warning: Technology without properly trained staff is ineffective. Budget time and money for comprehensive staff training to ensure your denial prevention system implementation succeeds.
| Role | Primary Responsibility | Key Success Metrics | Training Requirements |
| Practice Manager/Administrator | Overall strategy and performance monitoring | Denial rate under 8%, clean claim rate above 95% | Revenue cycle management certification |
| Patient Access/Registration Staff | Front-end prevention through accurate data collection | Eligibility verification accuracy >98% | Quarterly payer policy updates, customer service training |
| Prior Authorization Specialists | Obtaining timely authorizations and tracking | Authorization approval rate >90%, no missed deadlines | AAHAM Prior Authorization certification recommended |
| Medical Coders | Accurate code assignment and documentation review | Clean claim rate >95%, coding accuracy >98% | CPC/CCS certification + 36 hours annual CEUs |
| Billing and Collections Staff | Claims submission, denial tracking, appeals | Appeal success rate >60%, resolution time <30 days | AAHAM CRCS or similar revenue cycle certification |
| Denial Management Specialists | Root cause analysis and prevention strategies | Denial rate trending downward, prevention initiatives tracked | Cross-functional training in all revenue cycle areas |
Ready to Transform Your Practice’s Financial Performance?
At SovDoc, we help medical practice owners optimize their operations and maximize practice valuations through strategic improvements like denial prevention system implementation. Our healthcare M&A advisory team understands that strong operational metrics, including low denial rates, are essential for maximizing practice valuations. We work with practices across all specialties to ensure operational efficiency.
Contact SovDoc today to schedule a confidential consultation about your practice’s denial management system and learn how proper implementation can significantly increase your practice’s value and operational efficiency.



