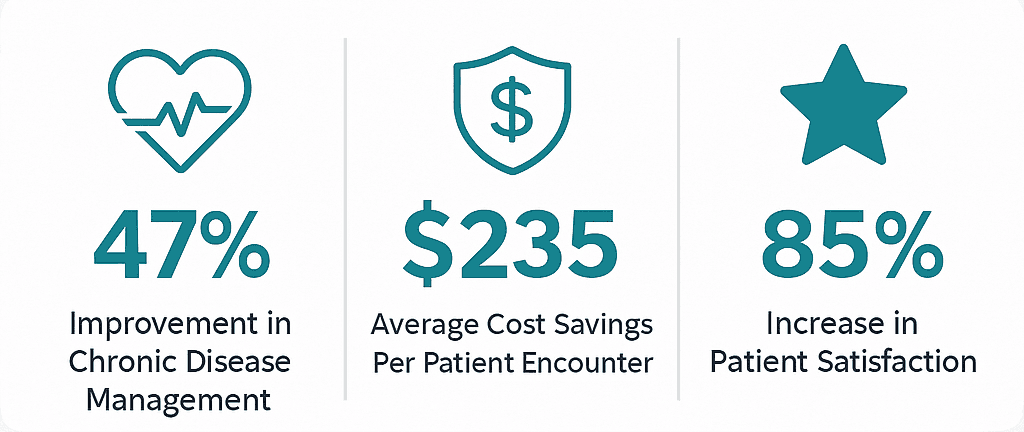
If you’re wondering how to bring virtual care into your practice, you’re in the right place. We know this transition can feel significant, but the benefits are compelling. Practices that effectively integrate virtual care are seeing a 47% improvement in chronic disease management and an average cost savings of $235 per patient encounter.
Our goal is to give you a practical roadmap. Successful integration isn’t just about adopting new technology; it’s about improving how you deliver care while strengthening the quality relationships your patients expect.
Insight: Virtual Care Integration Strategies aren’t about replacing your current practice model—they’re about enhancing it through strategic technology adoption that improves both patient outcomes and practice efficiency.
What Does Virtual Integration Really Mean for You?
Virtual integration in healthcare represents a coordinated approach that connects different aspects of your practice through technology-enabled partnerships and seamless information systems. Think of it as using technology to connect the different parts of your practice—your staff, workflows, and systems—so they work together seamlessly. Instead of the high capital investment required for new buildings or staff, you focus on coordinating care through shared technology.
This approach differs fundamentally from a traditional merger. You’re not physically consolidating; you’re creating connections that enhance what you already do. For your practice, this could mean ensuring your EHR system “talks” to your telehealth platform, allowing virtual visits to flow naturally into your existing documentation workflows. It’s about creating a unified patient experience, where scheduling, billing, and follow-up feel consistent, whether the visit is in-person or online.
Important: Virtual integration emphasizes coordination through patient management protocols and provider communication systems, rather than requiring massive capital investments in new facilities or staff.
How Does Virtual Integration Compare to Traditional Approaches?
| Traditional Integration | Virtual Integration |
|---|---|
| Requires physical facility mergers | Uses technology to connect existing locations |
| High capital investment in buildings/equipment | Lower upfront costs, focus on software/systems |
| Geographic consolidation needed | Can serve dispersed patient populations |
| Staff relocation often required | Existing staff work from current locations |
| Long implementation timelines (1-2 years) | Faster deployment (3-6 months) |
What Are Real Examples of Integration in Healthcare?
To make this less abstract, let’s look at how other practices have made this work through proven Growth Strategies.
Chronic Care Management Integration
Centura Health implemented a remote monitoring program for patients with chronic conditions like COPD and diabetes. By introducing the technology through doctors their patients already knew and trusted, they achieved an 85% increase in patient satisfaction. This shows that adoption is most successful when patients feel supported by familiar providers, not replaced by impersonal systems.
Centura Health’s approach demonstrates how effective virtual medical care strategy can achieve 47% improvements in chronic disease management while maintaining high patient satisfaction.
Virtual Urgent Care Integration
Third Eye Health developed a virtual urgent care program for skilled nursing facilities. Their system was able to resolve 91% of urgent issues within the facility, preventing costly and stressful emergency room visits and hospital readmissions. This model is particularly effective if you serve older populations or those with complex medical needs.
Comprehensive Platform Integration
Ascension Health’s comprehensive platform revealed that nearly 70% of virtual care patients would have otherwise used urgent care or emergency departments. This demonstrates how well-designed virtual care can redirect patients to more appropriate, cost-effective settings.
Cost Impact: These integration examples show how virtual urgent care can prevent up to 44% of unnecessary emergency department visits, saving an average of $235 per patient encounter.
How Is Integrated Care via Telehealth Beneficial to Your Patients?
When you successfully implement telemedicine integration, you can expect consistent benefits that impact both patient care and your practice’s sustainability.
Better Patient Outcomes and High Satisfaction
Virtual care is proven to improve clinical outcomes. Studies show that telehealth programs can increase treatment adherence by 67% and preventive care compliance by 73%. For chronic conditions, the results are particularly strong; diabetes care platforms have demonstrated enhanced patient engagement and improved HbA1c levels.
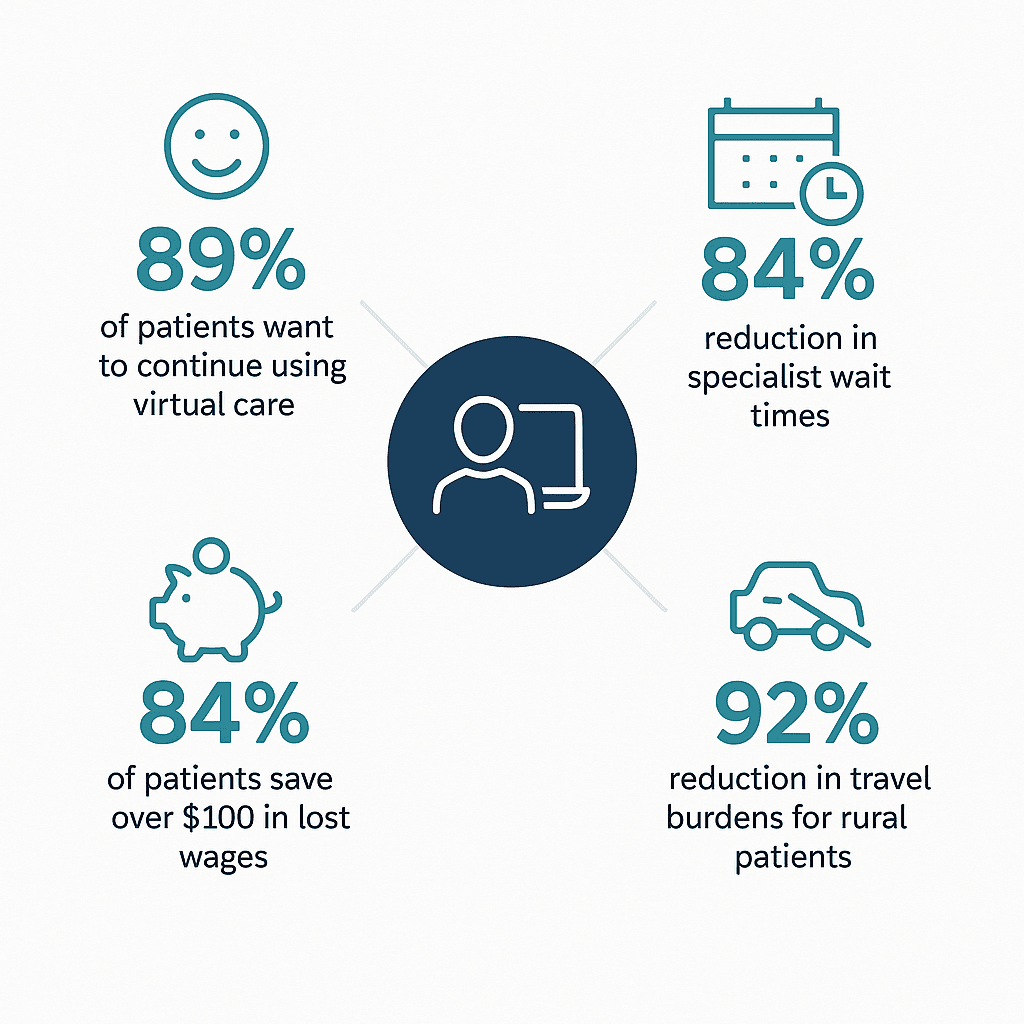
The satisfaction data is equally compelling. 89% of patients who use virtual care express a desire to continue, and the J.D. Power 2024 Telehealth Satisfaction Study shows an overall satisfaction score of 730 out of 1000 points.
Patient Benefit: Integrated care via telehealth eliminates 92% of travel burdens for rural patients and saves 84% of patients over $100 in lost wages per visit.
Significant Cost Savings and Efficiency Gains
The economic benefits are just as tangible. Beyond the average patient savings of $235 per encounter, practices see major efficiency gains:
- No-show rates drop dramatically: Psychiatry no-show rates have been shown to drop from a baseline of 19-22% down to as low as 4.4% with telehealth
- Reduced emergency utilization: 44% decrease in emergency department use
- Fewer readmissions: 63% reduction in hospital readmissions
- Faster specialist access: 84% reduction in specialist wait times
Imagine what that kind of reliability could do for your daily workflow and revenue predictability.
Enhanced Access and Health Equity
Virtual care integration provides compelling advantages for serving diverse patient populations across the United States. Treatment adherence improved by 67% across telehealth programs, while preventive care compliance rose by 73%. These improvements particularly benefit patients who might otherwise face barriers to consistent care.
Virtual care integration eliminates geographic barriers, with rural patients experiencing 92% reductions in travel burdens while maintaining equivalent clinical outcomes to in-person care.
How Do You Make Your Telemedicine Implementation Better?
Making telemedicine better requires a strategic focus on three critical areas: selecting the right technology, optimizing your workflow, and training your team. Here’s how successful practices are enhancing their virtual medical care strategy.
What Technology Features Are Essential?
When you evaluate platforms, there are several non-negotiable features for effective telemedicine integration:
- HIPAA-compliant, secure video conferencing that performs reliably even on lower bandwidths
- Integrated patient portal for scheduling and communication
- E-prescribing capabilities that connect with your pharmacy relationships
- Comprehensive EHR integration that allows for real-time documentation
- Multi-participant capabilities so family members can join consultations when appropriate
We find that a seamless connection to your existing EHR is one of the most critical factors for success.
Tip: The most successful telemedicine integrations prioritize interoperability standards like HL7 FHIR R4, which enable seamless data exchange across different EHR systems.
Beyond these basics, leading platforms offer advanced features that can further improve care and efficiency, including AI-powered diagnostic support, natural language processing for automated documentation, and predictive analytics that flag at-risk patients for early intervention.
What Are Your Technology Requirements by Practice Size?
| Practice Size | Internet Speed Needed | Platform Type | Monthly Cost Range |
|---|---|---|---|
| Solo Practice (1-2 providers) | 25 Mbps up/down | Cloud-based SaaS | $200-500 |
| Small Group (3-10 providers) | 50 Mbps up/down | Cloud with API integration | $500-1,500 |
| Medium Group (11-25 providers) | 100 Mbps up/down | Enterprise cloud solution | $1,500-5,000 |
| Large Group (25+ providers) | 250+ Mbps up/down | Custom enterprise platform | $5,000+ |
How Do You Optimize Your Workflow?
We understand that overhauling your workflow can seem daunting. The key is to minimize disruption by integrating digital tools into your existing processes. You can start by using pre-visit digital intake forms that patients complete at home. From there, look to automate post-visit processes, such as care plan distribution and medication management. Finally, an integrated billing system that processes virtual visits through your existing revenue cycle will save your administrative team significant time and effort.
Practices implementing comprehensive workflow optimization see 56-65% of their visits successfully delivered virtually without compromising quality.
What’s Your Strategic Action Plan?
Successfully implementing Virtual Care Integration Strategies requires systematic planning. Based on our experience with thousands of practices, here is a practical, four-phase roadmap.
Phase 1: Assessment and Planning (Months 1-2)
Your first two months should be dedicated to discovery:
- Evaluate your patient population to identify which services, like chronic disease management or routine follow-ups, would benefit most from virtual delivery
- Conduct a technology audit of your existing systems—your EHR, internet bandwidth, and billing software—to understand what integration will require
- Engage your staff early for insights into daily workflows and patient needs
Tip: Focus on services with the highest success rates for virtual delivery: chronic disease management (85% patient satisfaction increase), routine follow-ups, and behavioral health consultations.
Phase 2: Platform Selection and Setup (Months 2-4)
With your requirements defined, you can choose a platform that integrates well with your current systems. The best choice is often the one that enhances your capabilities, rather than forcing a complete overhaul. Before a full launch, pilot your chosen platform with a small group of providers and tech-savvy patients. This allows you to resolve any issues without disrupting your entire practice. During this time, also develop clear clinical protocols that define which visits are appropriate for virtual care.
Phase 3: Staff Training and Patient Education (Months 3-5)
Your team’s confidence is key, so provide comprehensive staff training that covers both the technology and your new clinical protocols. It’s helpful to role-play common scenarios, including how to handle technical difficulties. At the same time, create simple patient education materials that explain how to use the platform. We recommend starting with patients who are already comfortable with technology and then gradually expanding.
Phase 4: Full Implementation and Optimization (Months 4-6)
After your full launch, it’s crucial to monitor key performance indicators, such as appointment completion rates, patient satisfaction scores, and clinical outcome measures. This data will help you demonstrate success and identify areas for improvement. Collect patient and staff feedback regularly; you’ll find their insights are the best source for refining your workflows and enhancing the patient experience.
Practices following this systematic approach typically achieve their target utilization rates within 6 months while maintaining patient satisfaction scores ≥85%.
What Should You Measure to Track Success?
| Metric Category | Key Indicators | Target Benchmarks |
|---|---|---|
| Clinical Quality | Patient satisfaction, clinical outcomes, medication adherence | ≥85% satisfaction, improved disease metrics |
| Operational Efficiency | No-show rates, provider productivity, revenue per visit | <10% no-shows, maintained or improved productivity |
| Patient Access | Geographic reach, time to appointment, demographic diversity | Expanded service area, reduced wait times |
How Do You Navigate the US Regulatory Environment?
The regulatory landscape continues to evolve in favor of virtual care across the United States. CMS telehealth flexibilities continue through 2025, with over 250 services permanently covered by Medicare. Most private insurers have also expanded telehealth coverage, though you should verify policies with your major payers before implementing new programs.
For licensing, providers must be licensed in the state where the patient is located, though interstate compacts can simplify this process for many states. The Interstate Medical Licensure Compact now operates in 40+ states, making it easier to serve patients across state lines.
Regulatory Warning: All platforms must be fully HIPAA-compliant as the COVID-19 enforcement discretion period expired in August 2023. Controlled substance prescribing via telemedicine is currently allowed through December 31, 2025.
How Do You Get Started with Virtual Care Integration?
The virtual care integration opportunity represents one of the most significant transformations in modern healthcare. Practices that thoughtfully implement these programs are positioning themselves to provide better care while building more sustainable, efficient operations. Here are your immediate next steps:
- Assess your current technology infrastructure and identify any upgrades needed
- Survey your patients to understand their interest and tech comfort levels
- Research platform options that integrate with your existing EHR and practice management systems
- Connect with other practices in your specialty that have successfully implemented virtual care
- Consider expert guidance to navigate the complexities of integration
Getting Started: The question isn’t whether virtual care integration strategies make sense for your practice—it’s how quickly you can implement them effectively while maintaining the quality relationships your patients trust.
The technology and regulatory environments are more supportive than ever. Your patients are increasingly expecting virtual options, and the clinical evidence for its effectiveness continues to grow. 63% of patients express interest in continued telehealth utilization, and with $42 billion in annual national savings through telehealth, the economic case is clear.
Why Choose SovDoc for Your Virtual Care Integration?
As a leading medical M&A firm, SovDoc understands how virtual care capabilities impact practice valuation and operational efficiency. We’ve seen firsthand how practices with well-integrated virtual care programs command higher valuations and attract more qualified buyers. If you’d like to discuss how virtual care integration might work for your specific practice, or if you’re curious how these capabilities might impact your practice’s value in a potential sale, let us know. We’re always happy to help you explore these opportunities and develop strategies that support your long-term practice goals.
Practices with established virtual care programs are increasingly attractive to buyers, as they demonstrate adaptability, efficiency, and future-readiness in today’s healthcare market.



